In the design and manufacture of electromedical equipment and systems it is important to take into account electromagnetic compatibility (EMC). Also in the design and construction of health centers it is important to pay attention to the EMC among electromedical equipment. Health centers in general, such as medical offices or outpatient clinics, physiotherapy centers, clinics, and hospitals, contain to a greater or lesser extent electro-medical equipment, such as: electrosurgery units or electronic scalpels, short-wave diathermy application equipment, and laser hair removal equipment that produces high levels of electromagnetic interference (EMI). Likewise, they also use electromedical equipment that may be sensitive to EMIs such as: magnetic resonance imaging (MRI), cardiac ablation, ECG (electrocardiogram) and EEG (electroencephalography) equipment.
Despite the existence of rules and regulations, there is sometimes a low collaboration between the designers of hospital buildings and the operators of the equipment in health centers. A good understanding of EMC allows avoiding EMI problems and thus protecting the most critical medical systems.
Good electromagnetic design of electromedical equipment and good installation and maintenance practices, such as the use of zoning and safety distances between equipment and cables, can ensure that adequate EMF levels are achieved in healthcare facilities.
EMC problems in medical electrical equipment
Poor electromagnetic compatibility of electromedical equipment can be a serious problem in the healthcare environment. Although EMI is often considered a minor nuisance in medical facilities, there are documented cases where medical electrical equipment failures due to EMI have caused patient injury or even death. Some examples are the following:
In 1987, patient monitoring systems failed to raise an alarm due to EMI; two patients died as a result.
In 1992, in an ambulance, a patient connected to a cardiac-monitor-defibrillator died due to radio interference in communication with the hospital.
In 1993, a patient with a pacemaker went into ventricular fibrillation shortly after being scanned with a metal detector at an airport.
Some electric wheelchairs experienced erratic involuntary movements when approached by police or fire brigade radio equipment or handheld radio transmitters or mobile phones.
In the US, several cases of EMF problems related to: cardiac monitors, defibrillators, incubators, pacemakers, respirators and other electromedical equipment have been reported. Between 1994 and 2005 there were more than 405 problems, with 6 deaths, 170 injuries and 167 cases of malfunction. 72% of the cases were due to active devices implanted in the patient.
As in many other industries, the amount and complexity of electronics in hospitals and other medical settings is increasing year by year. Most manufacturers and designers of electromedical products have developed a good understanding of EMC and have applied it to their equipment. Pacemakers are a typical example, where their design with respect to their small size and their immunity to EMIs has improved in recent years. Pacemakers had failed in patients undergoing electrosurgery (as expected, as this situation is not recommended) and in other cases where patients kept mobile phones in their pockets close to their chests, a few centimeters from the pacemaker leads. subcutaneous Pacemakers today are very reliable, but they could still fail under very extreme conditions.
Power wheelchairs are another typical example: there are many stories of EMI problems with mobile phones or "walkie-talkies" causing wheelchair handling problems. In the 1990s the US Food and Drug Administration (FDA) investigated the problem and recommended that manufacturers change the design to have a minimum immunity of 20 V/m.
Legislation and standards in Europe
Before 1993, each European country had its own system for regulating the manufacture and sale of electromedical equipment. In order to unify legislation, the European Union introduced a series of directives, thus removing barriers to trade to promote the single market. Most electronic equipment is currently subject to the EMC Directive, 2004/108/EU. However, medical equipment is covered by one of three Product Specific Directives:
- The Medical Devices Directive (MDD) 93/42 / EEC.
- The Active Implantable Medical Devices Directive (AIMD) 90/385/EEC.
- The In Vitro Diagnostic Medical Devices Directive (IVDD) 98/79/EC.
In most cases, compliance is demonstrated thanks to compliance with the requirements of the specific standard IEC-EN 60601-1-2 (Medical electrical equipment. Part 1-2: General requirements for basic safety and essential performance characteristics. Collateral standard: Electromagnetic compatibility. Requirements and tests) and other standards such as CISPR 11 (Industrial, Scientific and Medical Equipment (ISM). Characteristics of radioelectric disturbances. Limits and methods of measurement). It is necessary to inspect the Declaration of Conformity, to identify whether the equipment has been tested to the relevant standards specific to its respective electromagnetic environment, before the equipment is placed in service. The use of many electronic equipment in the hospital environment, such as therapeutic equipment (equipment intentionally designed to emit electromagnetic energy) and diagnostic equipment, requires proper EMC management to ensure that potential EMIs are minimized to ensure that they can work together. no problem.
In addition to applying it to electro-medical equipment, EMC should be an integral part of the design process in planning the construction and facilities of healthcare facilities: electrical distribution in hospitals can be very varied and complex and it is important to ensure that its electrical distribution does not provide the means to propagate EMIs throughout the building. Standards such as EN 50147-2 provide guidelines for achieving good EMC practice.
Most medical equipment must comply with the MDD to be allowed to carry the CE Mark. Each member state designates a Competent Authority to apply and enforce the MDD Directive. The Competent Authority designates the Notified Bodies that must administer the conformity.
In Spain, Law 14/1986, of April 25, General Health, in its article 40, sections 5 and 6, attributes to the General State Administration powers for the regulation, authorization, registration or homologation, as appropriate, of medicines for human and veterinary use and other sanitary products and articles and those that, by affecting humans, may pose a risk to people's health; as well as to regulate and authorize the activities of those who are dedicated to the manufacture and import of the aforementioned products.
In turn, article 110 of said law entrusts it to assess the safety, efficacy and efficiency of technologies relevant to health and health care.
The use of many electrical medical equipment, in close proximity in the hospital environment, means that they encounter the same type of EMC problems as with other types of electronic products. However, there are some special characteristics of the hospital electromagnetic environment:
Failure of medical devices can lead to patient injury or death.
In the European Union, medical products are not covered by the EMC Directive. They are governed by the three specific product directives already mentioned.
Some equipment found in hospitals has been intentionally designed to emit electromagnetic energy during therapy. Other equipment, which may be located nearby, is designed to measure small physiological signals. This combination has a high probability of creating EMC problems.
In hospitals, there is the question of whether to ban or restrict the use of mobile phones because they can interfere with critical medical equipment.
Many medical devices connect directly to patients. For mains powered devices, the designer must ensure good insulation as well as guarantee EMC.
It is the responsibility of many companies and individuals to avoid EMF problems that can endanger patients:
- Equipment manufacturers and designers must ensure that medical electrical equipment complies with applicable emission and immunity limits.
- Hospital administrators, planners, and architects must keep potential sources of EMIs and potential victims separate.
- Users should be encouraged to report any serious EMI incident and make it easy for them to report it.
The IEC-EN 60601-1-2 Standard
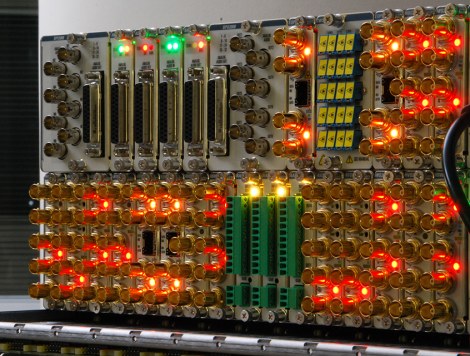
The IEC-EN 60601-1-2 standard applies to electro-medical equipment and systems used in medical applications. In common with the updated EMC standards, the IEC-EN 60601-1-2 standard defines limits for emissions and immunity levels. Test methods are defined by referring to various EMC standards shown in figure 1.
After years of debate, the standards have been updated to cover the frequencies used by mobile phones and other communication technologies, such as wireless local area networks (WLAN, Bluetooth, WIFI). It is worth noting that the standards specify EMC levels and how to test, but do not explain to designers and installers of systems and devices how to design them to achieve compliance.
Every designer of electrical medical equipment needs to take EMC into account through the IEC-EN 60601-1 and IEC-EN 60601-1-2 standards. Following these standards is a good guide for the EMC design of equipment. In addition, it is necessary to see the specific documents for the specific type of device that is being designed. The IEC has produced about 60 standards with special requirements. In addition to EMC and safety design requirements, there are strict manufacturing standards associated with the traceability of basic materials and manufacturing procedures. Quality control is an important part of the process, also for CEM.
Definitions and risks
From the perspective of the IEC-EN 60601-1 standard, electrical medical equipment is defined as: “Electrical equipment that has a part applied to the patient or has energy transfer to or from the patient or the detection of this type of energy towards or from the patient. This includes, for example, EEG monitors, image processing systems, ECG devices, vital sign monitors, and similar devices that connect directly to a patient's body.
Products that do not have direct connections to the patient's body are considered laboratory test devices and, in general, are regulated by the IEC-EN 61010 standard, which deals with the “Safety requirements for electrical equipment for measurement, control and use in laboratory”. Experimental medical devices must also meet these standards.
Risk management is also part of this process. The application of risk management to medical devices (ISO 14971: Medical devices. Application of risk management to medical devices) requires the breakdown of risks for all modes of operation and all failure scenarios. This results in a matrix of risk associated with the use of the device. The probability of occurrence should be ranked against the severity of the damage, such as any effect that is significantly detrimental and unlikely to occur.
The safety of isolation of patients is important in the design process. There are well-defined rules for the isolation of the patient and the operator of the equipment. This includes strict controls on leakage currents, applied voltages and the limits of energy to be transferred to the patient. Physical separations as well as electrical current leakage across dielectric jumpers to the patient and limitations on how power and data can be transferred across these jumpers are listed.
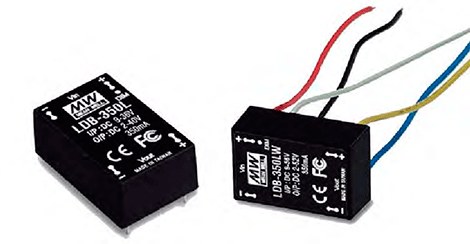
There must be no electrical current path between the patient and the system connected to the electrical network (IEC-EN 60601-1-1, Section 8). Any external power supply for an electromedical system must also comply with the standard. If an AC-DC power supply is placed inside the equipment, any step-down transformers must also comply with the standard.
Electromedical devices, when subjected to EMC tests, must not pass just 1 or 2 dB below the limit, but must have enough margin to respond correctly in all tests. Error messages, system resets, component failures, operating mode changes, programmable parameter changes, faulty patient information, and false alarms are not permitted. If any small performance degradation appears during the tests, the equipment must be redesigned so that this does not happen.
Radiated emission tests
In radiated emissions tests, the level of radiated EMIs generated by the equipment under test is measured. The emission limits imposed by the standards in frequency ranges from 30 MHz to 1 GHz must be complied with for all devices. But, depending on your design, you may have to face tests with frequencies up to 40 GHz up and 9 kHz down.
Medical electrical equipment and systems are classified as Class A or Class B and Group 1 or Group 2 under CISPR 11. Class A equipment is equipment suitable for use in all establishments other than domestic and is also equipment that They are directly connected to the public low-voltage electrical network, which supplies buildings used for domestic use. Class B equipment is equipment suitable for use in all establishments, including domestic establishments, and is also equipment that is directly connected to the public low-voltage power supply network, which supplies buildings for domestic use. Figure 2 summarizes this classification in a table.
Group 1 contains all ISM (industrial, scientific and medical) equipment in which conducted coupled RF (Radio Frequency) is intentionally generated or used, necessary for the internal operation of the same equipment. Therefore, its RF emissions are very low and are not likely to cause any interference in nearby electronic equipment. Most medical equipment belongs to Group 1. For example, RF body treatment equipment to produce an internal increase in the temperature of the fatty tissue of the dermis through electrodes in contact with the patient belongs to this group.
Group 2 contains all ISM equipment in which RF energy is intentionally generated or used in the form of electromagnetic radiation for material treatment, and spark erosion equipment. Nearby electronic equipment may be affected.
Some examples of Group 2 teams are:
- Medical Imaging Equipment (Magnetic Resonance Imaging Systems: (MRI))
- Therapy equipment (including short wave diathermy, short waves, ultra short waves and microwaves)
- Therapy equipment (hyperthermia)
- High frequency equipment and surgical systems (RF energy is applied to the patient)
Figure 3 presents the radiated emission limits for laboratory tests and on-site tests according to CISPR 11 for Group 1 equipment. Tables of limits for radiated emissions for Group 2 equipment 11 are more complex due to various equipment conditions and should be consulted directly in the CISPR XNUMX standard itself.
Conducted emissions tests
Conducted emissions tests are easier to perform than radiated emissions tests. These tests determine the level of EMIs that the device is sending to the mains line, following the CISPR 11 standard. The frequency range of the test is usually 150 kHz to 30 MHz.
If the device generates conducted EMIs, mains filters can be used to reduce its noise. Switch mode power supplies are the most common culprits for exceedances of conducted emissions limits.
Figure 4 shows the limits of conducted emissions for Class A devices. Figure 5 shows the limits of conducted emissions for Class B devices. It can be seen that the Class B limits for Group 1 equipment they are anywhere from 10 to 17 dB below the Class A limits, depending on the frequency range.
harmonic tests
Medical electrical equipment and systems with a nominal input current of less than 16 amps per phase must comply with IEC 61000-3-2 for harmonic distortion. The current harmonics sent into the grid determine what load current characteristics the device creates in the power grid. The alternating current voltage is ideally a sinusoid. If a resistive load is connected, the current is also a sinusoid. But if they connect active switching devices with non-linear responses, the load current may have a high harmonic content that needs to be filtered.
Medical electrical equipment and systems with an input current rating of less than 16 amps per phase must also comply with IEC 61000-3-3 for voltage fluctuations and flicker. Both IEC 61000-3-2 and IEC 61000-3-3 specify limits, test methods and test equipment. Power supply instabilities are examined using two separate tests: the power line flicker test (IEC 61000-3-3) and the voltage dip and interruption immunity test (IEC 61000-4-11). With these tests, it is verified how the complete equipment responds, including its power supply. The most critical test is a requirement where the mains supply voltage is reduced by 95% for 5 seconds. Essentially, the system is required to continue to function without failure. That is why many medical devices cannot use a simple power supply and need to add a battery. In some cases, the device may be able to continue to function properly due to the charge on its internal capacitors, but this depends on the power consumption of the device.
Two additional tests are applied to mimic non-ideal external power. For this, the IEC 61000-4-4 standard is applied, which applies an intermittent burst of impulses in the electrical or ground lines. Line surge immunity is tested using IEC 61000-4-5 where a wide range of waveforms is required. Both tests can apply up to ± 2 kV on the power and ground lines. Both tests require filtering and safety opening circuitry to keep the equipment operating correctly.
immunity tests
The immunity requirements are based on the IEC 61000-4-x series standards where x is 2, 3, 4, 5, 6, 8 and 11 (see again figure 1). Electrostatic discharge (ESD) tests are contained in the IEC 61000-4-2 standard. For electromedical equipment, they must comply with the test levels of ± 2 kV, ± 4 kV, ± 8 kV and ± 15 kV for air discharges and ± 2 kV, ± 4 kV, ± 6 kV and ± 8 kV for discharges by contact. Consideration must be given to how the discharges will flow to earth during the design in order to overcome this obstacle without difficulties. Acceptable performance during ESD testing of electro-medical devices is not simply obtaining equipment survivability from physical damage. It must also have correct functionality, without errors.
Radiated immunity criteria apply according to IEC 61000-4-3. The required level is 3V/m in equipment that is not dedicated to life support, vital in a frequency range of 80 MHz to 2,5 GHz for life support medical equipment and 10 V/m in the same range of frequencies for life support equipment. In RF immunity testing according to IEC 61000-4-3, the medical device is placed in a Faraday cage and subjected to RF emissions to see if it has problems in a noisy RF environment. This test includes electromagnetic fields that mimic cell phone transmissions. The vulnerability to these tests is due to sensitive broadband circuits, with high impedances and "long" connections that behave like antennas. To avoid problems of this type, impedances must be kept low and the bandwidth of any control circuitry, bias, or signal line limited. Figure 6 presents the details of the radiated immunity tests and the radio service bands that must be considered when carrying out these tests.
For electrical fast transient and burst tests, medical equipment shall have a test level of immunity of ±2 kV on alternating current (AC) power lines and ±1 kV on signal lines and interconnect cables. The test method is the one defined in the IEC 61000-4-4 standard that simulates the electrical noise generated by the switching of the switching relays.
Overvoltage tests are defined in the IEC 61000-4-5 standard. The requirements to be met are the test levels of ±0,5 kV, ±1 kV and ±2 kV between AC lines (phases) to ground and ±0,5 kV and ±1 kV between phases. This test simulates the side effects of lightning strikes.
The following immunity test is the RF Field Induced Conducted Disturbance Test according to IEC 61000-4-6. The test level is 3 volts (RMS) over a frequency range of 150 kHz to 80 MHz for non-life support equipment. The RF signal is modulated from 2 Hz to 1000 Hz, depending on the intended use of the equipment under test. 3 volts (RMS) is applied to life support equipment in the frequency range 150 kHz to 80 MHz, except in ISM frequency bands in that range where the equipment must comply with 10 volts (RMS). This test simulates cables acting as receiving antennas and the conversion of radiated fields into RF signals conducted through the cables.
The IEC 61000-4-8 standard determines the levels of immunity of magnetic fields, with levels of 1 A/m, 3 A/m, 10 A/m, 30 A/m and 100 A/m. This standard does not consider disturbances due to capacitive or inductive coupling in cables or other parts of the installation. The objective of this standard is to establish a common and reproducible basis for evaluating the performance of equipment when subjected to power frequency (50 Hz and 60 Hz) magnetic fields. To determine what needs to be done to pass this test, it is good to think about how the system would respond if it behaved like the secondary of a transformer. Improvement strategies include the use of twisted-pair cabling for common-mode EMI cancellation, the use of differential signals, and (rarely) splitting any large inductor into two parts in series with the wire they are attached to. physically connected, to produce the common mode voltage cancellation of the magnetic field in the two inductors.
The last immunity test is the test for voltage dips, short interruptions and voltage variations on AC input power lines, determined by the IEC 61000-4-11 standard. Non-life support equipment and systems that draw more than 16 amps per phase or have a power rating of 1 kVA are exempt from this test. All life support equipment must meet the criteria in figure 7. This is a test that simulates power fluctuations at the input of AC power lines that feed the power supplies for the complete electromedical equipment.
The electromedical device must pass all of these immunity tests, error free, and cannot provide false medical information or stop treatment. Alarms or error messages are also not acceptable. Figure 8 shows a summary table of all these immunity tests.
Other requirements of the IEC 60601-1-2 Standard
Medical electrical equipment containing RF transmitters or intentionally applying RF electromagnetic energy for diagnosis or treatment will be labeled with the non-ionizing radiation symbol shown in Figure 9. Figure 10 shows some examples of this type of equipment with non-ionizing radiation.
Medical electrical equipment and systems specified for use only in a shielded location will bear a label warning that they must be used only in the specified type of shielded location (for example, in rooms where X-ray machines are used).
In electro-medical equipment in which the exemption from tests on connectors specified in section 6.2.2.2 applies. c) of the IEC 60601-1-2 standard, the symbol of the IEC 60147-5134 standard shown in figure 11 must be used, for ESD sensitivity.
This symbol will be placed adjacent to each connector exempt from testing.
Regarding the accompanying documents, in the instructions for use, all electro-medical equipment and systems must include the following:
A statement that the electrical medical equipment requires special EMC precautions and needs to be installed and put into service in accordance with the EMC information provided in the accompanying documents.
A statement that portable and mobile RF communications equipment can affect medical electrical equipment.
In the technical description, the accompanying documents on all electro-medical equipment and systems will include the following:
A list of all the cables with their maximum lengths (if applicable), transducers and other accessories with which the manufacturer of the equipment and the electromedical system declares compliance with the requirements of the standards. It is not necessary to list accessories that do not affect compliance with the requirements of these standards. Accessories, transducers, and cables can be specified generically (eg, standard shielded cable, load impedance) or specifically (eg, by manufacturer and model or part number).
A warning that the use of accessories, transducers, and cables other than those specified, with the exception of transducers and cables sold by the equipment manufacturer as replacement parts, may result in increased emissions or decreased immunity of the equipment electromedical.
A warning that medical electrical equipment should not be used adjacent to or stacked with other equipment and that if adjacent or stacked use is necessary, the equipment should be observed to function properly in the configuration in which it is to be used.
A justification for each immunity level that fails to meet the required level for that immunity test. These justifications must be based solely on physical, technological or physiological limitations that prevent compliance with the test level of the IEC 60601 standard.
The benefits of the electromedical equipment that determine its essential functioning.
Conclusions
A good understanding of electromagnetic compatibility allows avoiding EMI problems and thus protecting the most critical electro-medical systems.
The optimal electromagnetic design of electromedical equipment and good installation and maintenance practices, such as the use of zoning and safety distances between equipment and cables, can ensure that adequate EMF levels are achieved in health centers.
The IEC-EN 60601-1 and IEC-EN 60601-1-2 standards apply to electrical medical equipment and systems.
These standards define how to manage risk analysis and limits for emissions and immunity levels in electromagnetic compatibility testing, making reference to various EMC standards.