The ability to see electrical connections inside a patient's body and determine the cause of disease without causing death or serious injury has long been a medical dream. Any type of surgery is an invasive process that puts considerable stress on the body. Specifically, the cardiovascular, respiratory, excretory, and immune systems are put at risk, and the body's ability to maintain homeostasis is compromised. Therefore, if surgery is essential, the use of minimally invasive surgery (MIS) techniques to limit the size and number of incisions made is extremely beneficial to the patient.
MIS offers many advantages over traditional open surgery. Wounds caused by MIS procedures are smaller, which helps shorten recovery times and leave less visible scarring. Patients recover faster, so they can leave the hospital earlier and free up beds for other patients. Many patients experience less color after MIS and therefore require less postoperative medication.
Research firm Market & Markets forecasts that by 2025 the global turnover generated by MIS-related equipment will amount to about $32.700 billion per year. The fields of expertise in which it is proving particularly valuable are thoracic, orthopedic, urologic, vascular, gynecologic, and neurologic surgery, as well as interventional cardiology.

Figure 1: Minimally invasive surgery has improved recovery times for patients. Source: Bork/Shutterstock.com
The first investigations leading to modern MIS took place in the early 1980s with the introduction of various types of electrosurgical instruments (catheters, endoscopes, laparoscopes, arthroscopes, etc.) that were critical to its continued technological advancement. It is currently estimated that more than 90% of all surgeries can be performed with MIS. These include appendectomy, tubal ligation, cholecystectomy, gastric bypass and gastric banding, heart valve repair, myomectomy, hysterectomy, arthroscopy, prostatectomy, spinal fusion, and bariatric procedures. In the future, surgeons will be able to use MIS more frequently as the technology behind it becomes more sophisticated.
Continual innovations in electrosurgical instruments will allow them to incorporate high levels of functionality and consequently these instruments will be more effective. It will also open up opportunities to apply MIS to the treatment of a broader range of health disorders and medical problems. However, to retain their “non-invasive” properties, the surgical devices used in the procedures must be very small in size. This has far-reaching implications for the electronics they integrate, not only for their components (microsensors, actuators, power management ICs, etc.) but also for the cabling that supplies the data signals and the feeding.
The cabling required in these designs has not received much attention to date in terms of footprint, but the requirement for smaller form factors, coupled with the addition of functional elements, places space constraints on instrument designs. . As a consequence, it is necessary to change the way of wiring medical devices.
Until now, conventional electrosurgical instrument designs have used electrical interconnects based on microwiring technology, the cables of which must generally be combined together in bundles of about 600µm in diameter. In addition to their thickness, microleads have other drawbacks that medical engineers should be aware of, such as their stiffness, which makes them less practical for unusually shaped housings.
As the density of electronic content embedded in modern electrosurgical instruments continues to increase, the interfaces that interconnect everything will also need to evolve. Flexible Printed Circuits (FPCs) represent a viable option to replace microcables. FPCs allow substantial space and weight savings, as well as offering high levels of signal integrity and long-term operational reliability. Thanks to all this, the use of FPCs has become widespread in numerous wearable and implantable medical devices that are used in the monitoring, regulation and assistance of vital physiological processes such as pacemakers, hearing aids and blood glucose meters. Other advantages are the possibility of bending and shaping them in order to adapt them to the dimensions of the casing that contains them. The composite material structure of the FPCs provides them with considerable mechanical robustness so that their operation is effective even when they are much thinner.
With an FPC it is possible to implement conductive tracks with a width of only 25μm. With a total interconnect thickness (including electrical insulation and shielding layers) of less than 50μm, this solution is slightly thinner than a human hair. As a result, a single FPC can replace up to 12 microcables, which not only saves space but also reduces complexity when wiring the instrument. It is also worth noting that additional cost savings are achieved by replacing multiple microcable connections with a single FPC as this reduces the bill of materials and cost involved in wiring the product.
Although FPCs offer an attractive alternative to microleads, there remains a significant hurdle to overcome for their large-scale fabrication and introduction into devices for MIS procedures. Manufacturing techniques have limited the length of the FPC. Thus, most FPC manufacturers can achieve lengths of around 0,6m and only a few companies offer solutions up to 2m. This has undoubtedly had a detrimental effect on their ability to meet the design criteria of medical device OEM manufacturers.
Simply put, there are a multitude of MIS application examples where longer cabling solutions are needed. For example, catheters used in cardiac procedures require a minimum length of 1,1m for proper use by medical personnel. Similarly, in procedures such as interventional neuroradiology, the length of the wiring is 2m.
Thanks to its proprietary IHT (Improved Harness Technology™), Trackwise is the only one that manufactures multilayer FPCs of any length. This revolutionary manufacturing technique provides medical OEMs with a lighter weight, smaller, and unlimited length alternative to current solutions.
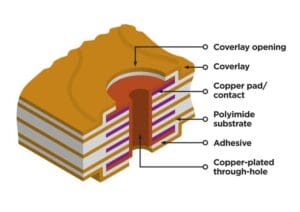
Figure 2: Example of ultra-thin IHT interconnect.
Source: Trackwise
Unlike conventional methods applied to FPC production, IHT employs a fully proprietary dynamic process that is based on advanced roll-to-roll electrolamination techniques. Thanks to these techniques it is possible to obtain FPC of any length, also guaranteeing its continuous reliability and repeatability and reducing the associated unit costs. The flat shape of IHT interconnects allows them to be attached within the structure to which they are mounted, thus reducing the physical space they occupy.
With IHT, Trackwise is able to produce FPCs in lengths far beyond those offered by other suppliers, enabling medical OEM manufacturers to have a large-scale, economical supply of FPCs suited to their specific application requirements. This is certain to be valuable in the design and commercialization of the next generation of instruments for MIS.